For nearly two decades, Able Flight, a remarkable nonprofit organization, has been on a mission that defies convention and breaks down barriers. With unwavering dedication, they have been empowering people with disabilities to take to the air, transforming their aspirations into soaring realities. Join us in this reading as we take flight alongside these extraordinary individuals, soaring through the skies of determination, courage, and boundless potential.
Nationwide, only 25 to 30 percent of student pilots successfully complete their training and earn a license. At Able Flight, a nonprofit that’s been training pilots with disabilities for nearly 20 years, the success rate is above 95 percent.
“And we train to a really high level,” says Charles Stites, the organization’s founder and executive director. “We don’t train to the FAA minimum for that certificate. We actually double the required number of hours.”
Able Flight students succeed for a lot of reasons, Stites explains. For one thing, it doesn’t cost anything—everyone who’s accepted into the program gets a full scholarship. Then there’s the sky-high caliber of instruction, which includes eight weeks of onsite flight training at the nationally renowned Purdue University School of Aviation. “But the main thing is that people come in highly motivated,” says Stites. “They get really good instruction, and we pair people up with mentor pilots who share their disability.”
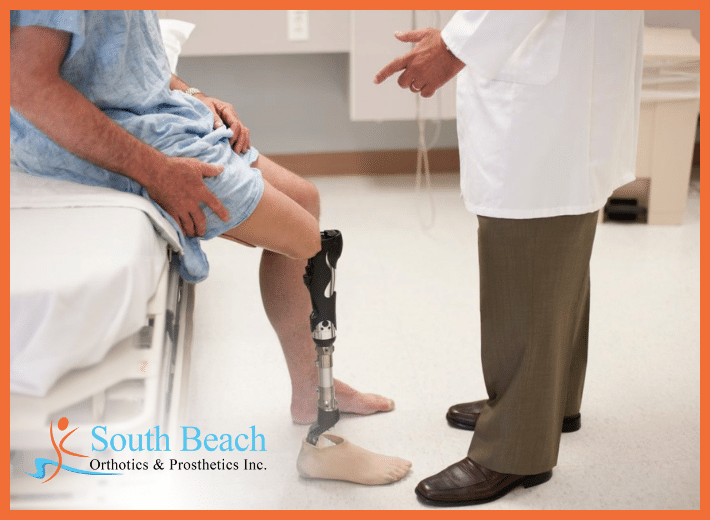
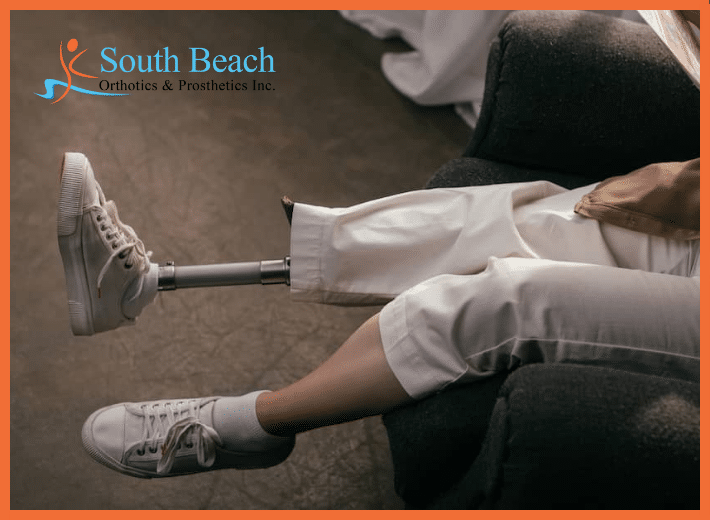
Those who earn their wings through Able Flight acquire far more than a new hobby. They come away with an altered self-perception, full of confidence and a newfound sense of freedom. Dozens of amputees have completed the program, including one (Jessica Cox) who made headlines as the first pilot to become licensed as a bilateral upper-limb amputee. Alumni have come from all over the country and included wounded veterans, college students, congenital amputees, and people who held a pilot’s license before becoming disabled and wish to return to the air.
“By the time someone finishes Able Flight, they don’t see themselves as a a pilot with a disability,” says Stites. “They just see themselves as a pilot.” Earlier this month we spoke with Stites about the program, which recently opened its application cycle for the class of 2024. If you’re interested in applying, you can get more info (including photos and videos) at Able Flight’s website. You have until December 31 to submit an application. Our conversation is lightly edited for clarity and length.
Tell me about the origins of Able Flight.
I’ve been a pilot for over 40 years, and I was an aviation writer and photographer for US and European magazines. Back around 2005, the FAA changed the rules for medical qualification and created a new category that increased opportunities for people who previously would have found it difficult, if not impossible, to qualify for a pilot’s license.
At around the same time, the US distributor for an Italian-made airplane came up to me at a big aviation event, and said, “You need to look at these new adaptive controls for flying. Can you get an article into your magazine?” I said, “It won’t be an article until you get them in an airplane and somebody’s using them.” He said they would be in airplanes in the fall, and we’ll see if we can do something then.
About a week later, it hit me that we have this incredible opportunity. We have this new FAA regulation that’s creating a new category of pilots, and we have an adaptive airplane that can be flown by those pilots that’s due to arrive in a few months. I decided it was time to change everything I’m doing. And so I incorporated Able Flight as a nonprofit in 2006.
What was the FAA rule that changed?
Prior to the advent of the sport pilot rule, people would go to an FAA medical examiner for a physical exam before they went for their pilot’s license. If they had what the FAA considered a disability, they would have to get further testing. Well, that could sometimes take six months to a year, depending on the nature of the disability. It might require a whole series of tests. A lot of people just gave up at that point, because you’re going to spend a couple thousand dollars or more, and you’re discouraged by the fact that you just keep constantly having to prove yourself fit to fly.
The sport pilot rule was based on the success of people who were trained to become glider pilots. They did studies and found that people were not crashing gliders because of a medical disability. And all you need for that is a valid driver’s license. So now you no longer have to prove yourself to a medical examiner. You just have to prove yourself to your flight instructor.
Like any nondisabled flight student.
And on the personal side, I’m married to someone that has multiple sclerosis. Most people wouldn’t know that she does, but she definitely feels the effects. And the idea just grew on me that, you know, we have this wonderful thing we can all do. We can fly. So why not expand that opportunity to people who would never have thought of themselves as candidates to do that.
Elaborate on that phrase for me, “this wonderful thing we can do.” What is the allure of taking to the skies? What impact has it made on your life, and what’s the impact for people who go through your program?
Well, for me personally, it sounds like a cliche, but it really is true that when you leave the earth, your ordinary cares don’t get to intrude much. It’s like you’re in your own little bubble, your own place. And anything that seems petty or harsh or rough to deal with, it tends to go away.
I came from limited circumstances and I never thought I’d get to fly. I thought that opportunity was beyond me. But when I got old enough and took my first lesson, I was hooked. I became a private pilot in about 1980, added an instrument rating some years later, and started doing aviation writing and photography. In aviation journalism, there are people who do really well writing about technology and advancements, but my heart was never really in that. I loved writing about people, and how flying changed their lives.
We set up Able Flight as a 501(c)3 in 2006. I started raising funds using connections I had in the industry, and by 2007 we were training people. And then in 2010, I proposed to Purdue University, which is one of the premier flight-training universities in the United States, that they become our training partner. I honestly had no idea that they were gonna say yes, and they said yes immediately. So we’ve been with them ever since. We’ve been able to grow it to the point where we now have 89 people who are licensed, some with more than one license or certificate.
How do you think Able Flight changes the lives of amputees who go through the program?
When we first started out, I would talk about the challenge and freedom of flight. But as we started getting more people through the program, and I would talk to them about their experience, they almost never said challenge. They said freedom. Becoming a pilot freed them from the restrictions and boundaries of their day-to-day lives. We all have them in some way or another, and for some people the restrictions are more impactful. But that’s what I would hear: Freedom, freedom, freedom.
The other thing I’ve found is that people would start to see themselves as just a pilot. And that’s something I’ve always strongly encouraged: You’re not a pilot with a disability; you’re a pilot. You’re an aviator. You’re flying the airplane according to the same rules and the same responsibilities as everyone else. You’ve learned the same skills, met the same requirements, passed the same tests, and you’re held to the same standards. The only difference is that you might be using some different controls based on the nature of a disability. But that doesn’t make any difference. To any person that hears you on the radio, you’re just a pilot. So it’s really a leveling kind of thing. It’s an equality thing.
If you’re good enough to do it, you’re good enough to do it.
Absolutely. You’re flying the plane exactly the same as any pilot, regardless of physical capabilities or body shape. People have designed adaptive controls—we’re in the middle of one of those projects right now, in fact, and it’s pretty exciting. We’re trying to get another airplane adapted, and this particular plane is made here in the United States. But ultimately, the person adapts themselves to the airplane. People who have less range of motion, for example, they’ll figure out another way to get the leverage they need to work all the controls. And they’ll do it on their own.
We have all these wonderful instructors who volunteer to teach Able Flight pilots, and at first some of them worry about whether or not a person is going to be able to pull something off. I’ve seen that happen so many times now. This year, specifically, I remember having that conversation over a gentleman named Bobby Dove. Bobby’s a wounded veteran, and he’s missing both limbs on the right side of his body. And so Bobby and I and his instructor, Cameron, were at one of the airplanes on the very first day of orientation, before they started flying. Cameron and I exchanged a glance and went, “Oh boy, how’s this gonna work?” Does he maybe come up with a strap on the rudder pedals, so by pulling and pushing, it would make the other pedal move and you could get them in motion? It turns out that airplane doesn’t work that way. It didn’t have that kind of range of motion. So that didn’t work.
I just told Cameron: Let Bobby figure it out. He’s an expert in his own life; he knows how to get things done. So just let him see if he can come up with a solution, because we’ve seen that happen a number of times. Sure enough, three or four days later, Bobby’s doing his first few flights, and he’s doing great. He was ready for his solo flight earlier than all but one of the other students this year.
That’s why I just tell the instructors not to worry. People always find a way. They come up with these clever adaptations and creative solutions. And that’s one of the wonderfully rewarding things about this program.
Let’s focus on a few nuts and bolts of the program. What’s the duration, how many of those hours are in the air versus in the classroom or simulator, what type of airplanes you’re flying, that sort of thing.
We’ll start with the certificate that everyone trains for. It’s called a sport pilot certificate, which is basically one level below private pilot. But don’t let that fool you. These are very sophisticated airplanes, and the way we do the training is really right up to private-pilot levels. Matter of fact, we’ve had a number of people that have gone on to get the private pilot certification.
We use light sport aircraft, which are very sophisticated airplanes now. They typically cost $120,000 to $175,000, and they can be flown coast to coast, they can be flown in controlled airspace around big cities and so on. They’re not limited.
The students start by doing about three months of online study to prepare them for the FAA written exam, which is technically called the “Knowledge Test.” And that’s a good word for it, because there’s a huge amount of knowledge you have to absorb. That’s one of the things a lot of people don’t understand about learning to fly. You probably spend two or three hours on the ground, studying, for every hour you spend in the airplane. So they do months of preparation in advance before they depart for training. We give them tutoring during that time, and even some live online sessions with an instructor. They take the Knowledge Test at a local testing center near where they live.
Around the third week of May they arrive at Purdue. They get their own room in a dorm on campus, and obviously it’s an accessible room. They start flying about the second day, and they fly every day, seven days a week, for six to seven weeks, weather permitting. Often twice a day. The only time they don’t fly is when weather doesn’t allow it. It’s very intensive, very demanding. It’s really more of a bootcamp thing for aviation. And people love it. They go through the experience and say it’s the best thing they’ve ever done. But they also know they earned that license, because they work really, really hard. They’ll uniformly say, no matter how many times you tell them in advance, “I didn’t realize it was gonna be this hard.” It’s mentally and physically demanding. But there’s an amazing amount of satisfaction that comes with it.
The two biggest milestones are the first day they fly solo, which typically happens between a third and halfway through, and then there’s the check ride, when you go out with an FAA examiner—basically the same as when you go out for your driver’s license. First you have to pass an oral exam, and then you go up in the airplane and demonstrate a set of maneuvers. Everybody in our program does really well, because they’ve gotten really good instruction. The instructors don’t send them off for the check ride until they’re ready. Everybody we’ve ever sent for a check ride has passed. And that’s another remarkable statistic.
One of the things I always stress for anybody who wants to take part in this is that because you earn it, you’re welcomed into the world of aviation as an equal with everyone else. It’s a very welcoming environment, and they’re always looking at new things and new technologies. It’s a great community to be in.
Ready to take the next step towards a more mobile and fulfilling life? Discover the possibilities with our state-of-the-art prosthetic solutions. Together, we can explore the world of enhanced mobility and independence that awaits you. Contact us today at (888) 819-4721. Follow us on Instagram @SouthBeachOP for more tips on prosthetic care.
Reference: [https://livingwithamplitude.com/amputee-airplane-pilot-able-flight/]